Even with the USCGC TAHOMA airlifts, the hospital remained under-
utilized, particularly tragic given the incredible number of victims and
the gravity of their wounds. The injured had been removed from the
rubble within hours or even days of the disaster. Then they waited
even longer for helicopter transport. The delay resulted in severe
secondary complications, posing an even greater challenge for the
emergency medical teams. “Our surgeons have begun to speculate
on the numbers of people languishing in Port au Prince that have
perished since the few flights that have come to Milot.” wrote Tim
Traynor. “Septic poisoning and other very curable infections are taking
their toll on the innocents. Right now, gangrene is moving faster than
evacuation transportation.”
CRUDEM staff and board
members conducted a massive email, phone and media
campaign about the hospital and its capabilities. “We
need patients!” appealed Denise Kelly, Executive Director
of CRUDEM/ Hôpital Sacré Coeur. “We have top notch
facilities and surgeons on-site anxiously awaiting more
patients. People are dying in Port au Prince unnecessarily.
Bring them to us! Bring them to us however you can.
Stop this tragedy. Stop this unnecessary suffering and
death.” The appeals worked. The U.S. Navy joined in
the airlifts to Milot, buses and cars from Port au Prince
managed the grueling trip by land and delivered seriously
injured patients to Hôpital Sacré Coeur. The USS Comfort,
stationed in Port au Prince Harbor, sent patients to Milot.
The patient count increased daily.
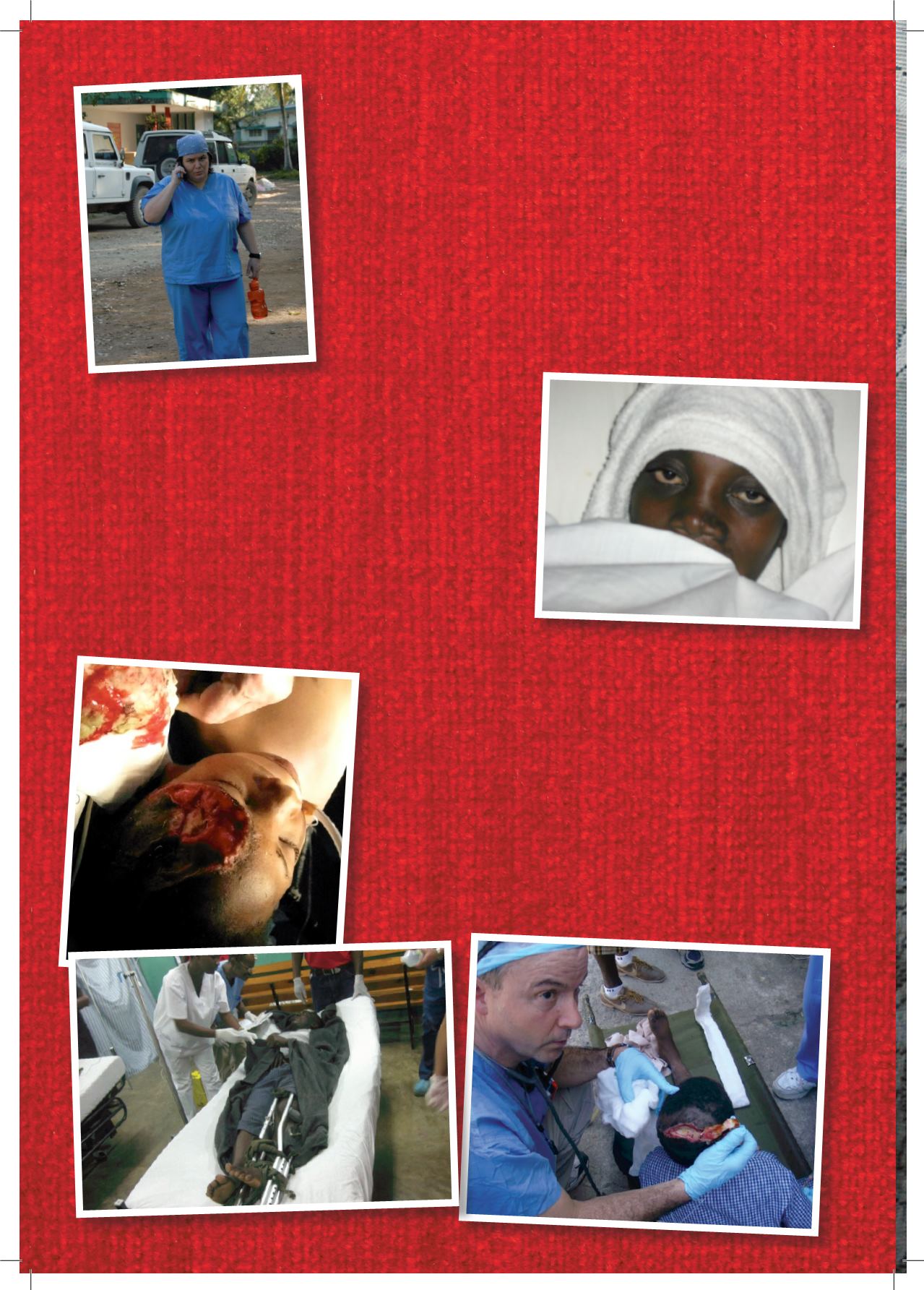
On Monday, January 18, a team of three orthopedic surgeons
and nurses arrived by private jet from Florida, its use donated
by Clean the World. Dr. John Lovejoy, Jr. and his son John,
a pediatric orthopedist from Washington, D.C. quickly
joined the Fletcher team and came up with a plan to divide
the labor. The orthopedists spent the rest of the day in the
operating room as they cleaned open wounds, set fractures,
and performed more amputations in a few days than they had
throughout their careers. As patients streamed in, additional
operating rooms were needed. Dr. Pitera and Raphael, a Sacré
Coeur orderly, quickly converted the delivery room into a third
operating room. The third room had no OR lights and after
dark teams used a gooseneck lamp and flashlights. That day
alone the Fletcher and Lovejoy teams did 26 operative cases and
procedures that required anesthesia or conscious sedation.















